Explanation of Balance Billing
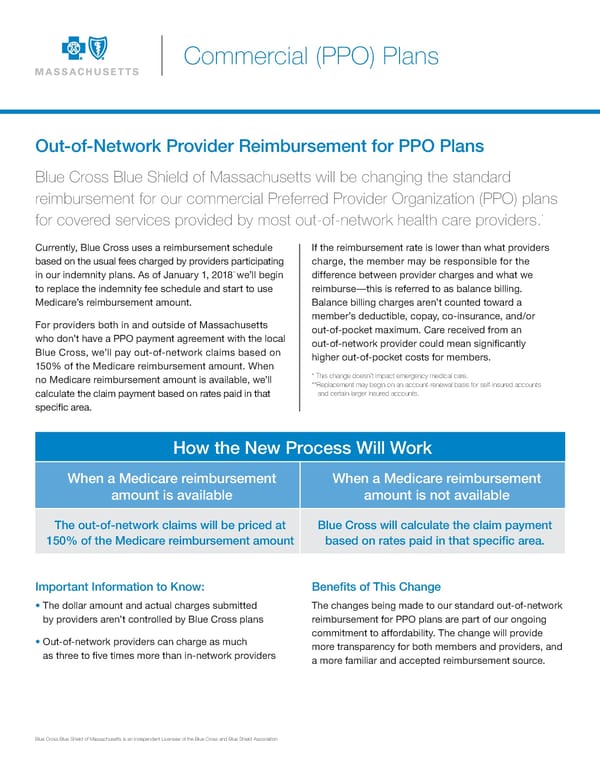
Commercial (PPO) Plans Out-of-Network Provider Reimbursement for PPO Plans Blue Cross Blue Shield of Massachusetts will be changing the standard reimbursement for our commercial Preferred Provider Organization (PPO) plans * for covered services provided by most out-of-network health care providers. Currently, Blue Cross uses a reimbursement schedule If the reimbursement rate is lower than what providers based on the usual fees charged by providers participating charge, the member may be responsible for the ** in our indemnity plans. As of January 1, 2018 we’ll begin difference between provider charges and what we to replace the indemnity fee schedule and start to use reimburse—this is referred to as balance billing. Medicare’s reimbursement amount. Balance billing charges aren’t counted toward a member’s deductible, copay, co-insurance, and/or For providers both in and outside of Massachusetts out-of-pocket maximum. Care received from an who don’t have a PPO payment agreement with the local out-of-network provider could mean signi昀椀cantly Blue Cross, we’ll pay out-of-network claims based on higher out-of-pocket costs for members. 150% of the Medicare reimbursement amount. When no Medicare reimbursement amount is available, we’ll * This change doesn’t impact emergency medical care. **Replacement may begin on an account-renewal basis for self-insured accounts calculate the claim payment based on rates paid in that and certain larger insured accounts. speci昀椀c area. How the New Process Will Work When a Medicare reimbursement When a Medicare reimbursement amount is available amount is not available The out-of-network claims will be priced at Blue Cross will calculate the claim payment 150% of the Medicare reimbursement amount based on rates paid in that speci昀椀c area. Important Information to Know: Bene昀椀ts of This Change • The dollar amount and actual charges submitted The changes being made to our standard out-of-network by providers aren’t controlled by Blue Cross plans reimbursement for PPO plans are part of our ongoing commitment to affordability. The change will provide • Out-of-network providers can charge as much more transparency for both members and providers, and as three to 昀椀ve times more than in-network providers a more familiar and accepted reimbursement source. Blue Cross Blue Shield of Massachusetts is an Independent Licensee of the Blue Cross and Blue Shield Association.
 Explanation of Balance Billing Page 2
Explanation of Balance Billing Page 2