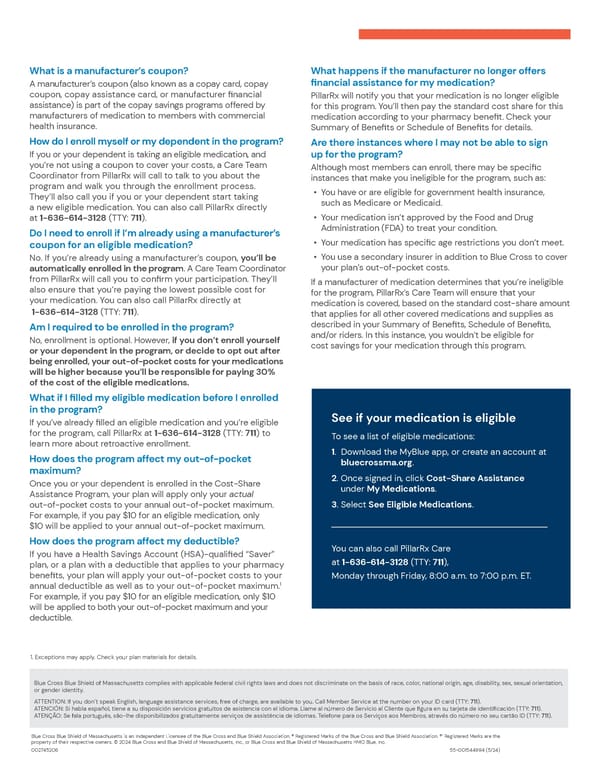
What is a manufacturer’s coupon? What happens if the manufacturer no longer offers financial assistance for my medication? A manufacturer’s coupon (also known as a copay card, copay coupon, copay assistance card, or manufacturer financial PillarRx will notify you that your medication is no longer eligible assistance) is part of the copay savings programs offered by for this program. You’ll then pay the standard cost share for this manufacturers of medication to members with commercial medication according to your pharmacy benefit. Check your health insurance. Summary of Benefits or Schedule of Benefits for details. How do I enroll myself or my dependent in the program? Are there instances where I may not be able to sign If you or your dependent is taking an eligible medication, and up for the program? you’re not using a coupon to cover your costs, a Care Team Coordinator from PillarRx will call to talk to you about the Although most members can enroll, there may be specific program and walk you through the enrollment process. instances that make you ineligible for the program, such as: They’ll also call you if you or your dependent start taking • You have or are eligible for government health insurance, a new eligible medication. You can also call PillarRx directly such as Medicare or Medicaid. at 1-636-614-3128 (TTY: 711). • Your medication isn’t approved by the Food and Drug Do I need to enroll if I’m already using a manufacturer’s Administration (FDA) to treat your condition. coupon for an eligible medication? • Your medication has specific age restrictions you don’t meet. No. If you’re already using a manufacturer’s coupon, you’ll be • You use a secondary insurer in addition to Blue Cross to cover automatically enrolled in the program. A Care Team Coordinator your plan’s out-of-pocket costs. from PillarRx will call you to confirm your participation. They’ll If a manufacturer of medication determines that you’re ineligible also ensure that you’re paying the lowest possible cost for your medication. You can also call PillarRx directly at for the program, PillarRx’s Care Team will ensure that your medication is covered, based on the standard cost-share amount 1-636-614-3128 (TTY: 711). that applies for all other covered medications and supplies as Am I required to be enrolled in the program? described in your Summary of Benefits, Schedule of Benefits, No, enrollment is optional. However, if you don’t enroll yourself and/or riders. In this instance, you wouldn’t be eligible for or your dependent in the program, or decide to opt out after cost savings for your medication through this program. being enrolled, your out-of-pocket costs for your medications will be higher because you’ll be responsible for paying 30% of the cost of the eligible medications. What if I filled my eligible medication before I enrolled in the program? See if your medication is eligible If you’ve already filled an eligible medication and you’re eligible for the program, call PillarRx at 1-636-614-3128 (TTY: 711) to To see a list of eligible medications: learn more about retroactive enrollment. How does the program affect my out-of-pocket 1. Download the MyBlue app, or create an account at maximum? bluecrossma.org. Once you or your dependent is enrolled in the Cost-Share 2. Once signed in, click Cost-Share Assistance Assistance Program, your plan will apply only your actual under My Medications. out-of-pocket costs to your annual out-of-pocket maximum. 3. Select See Eligible Medications. For example, if you pay $10 for an eligible medication, only $10 will be applied to your annual out-of-pocket maximum. How does the program affect my deductible? You can also call PillarRx Care If you have a Health Savings Account (HSA)-qualified “Saver” at 1-636-614-3128 (TTY: 711), plan, or a plan with a deductible that applies to your pharmacy benefits, your plan will apply your out-of-pocket costs to your Monday through Friday, 8:00 a.m. to 7:00 p.m. ET. 1 annual deductible as well as to your out-of-pocket maximum. For example, if you pay $10 for an eligible medication, only $10 will be applied to both your out-of-pocket maximum and your deductible. 1. Exceptions may apply. Check your plan materials for details. Blue Cross Blue Shield of Massachusetts complies with applicable federal civil rights laws and does not discriminate on the basis of race, color, national origin, age, disability, sex, sexual orientation, or gender identity. ATTENTION: If you don’t speak English, language assistance services, free of charge, are available to you. Call Member Service at the number on your ID card (TTY: 711). ATENCIÓN: Si habla español, tiene a su disposición servicios gratuitos de asistencia con el idioma. Llame al número de Servicio al Cliente que figura en su tarjeta de identificación (TTY: 711). ATENÇÃO: Se fala português, são-lhe disponibilizados gratuitamente serviços de assistência de idiomas. Telefone para os Serviços aos Membros, através do número no seu cartão ID (TTY: 711). Blue Cross Blue Shield of Massachusetts is an Independent Licensee of the Blue Cross and Blue Shield Association. ® Registered Marks of the Blue Cross and Blue Shield Association. ®’ Registered Marks are the property of their respective owners. © 2024 Blue Cross and Blue Shield of Massachusetts, Inc., or Blue Cross and Blue Shield of Massachusetts HMO Blue, Inc. 002745206 55-001544994 (5/24)
 Massachusetts Cost-Share Assistance Program Overview Page 1
Massachusetts Cost-Share Assistance Program Overview Page 1 