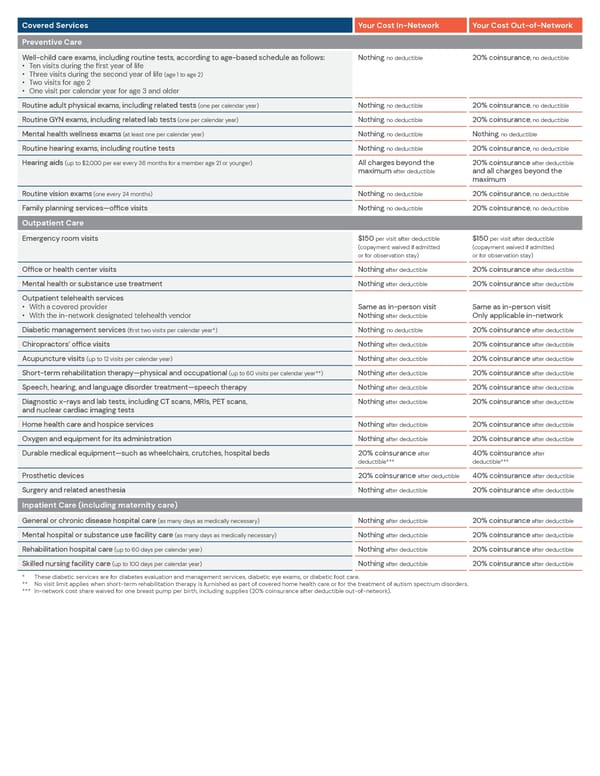
Covered Services Your Cost In-Network Your Cost Out-of-Network Preventive Care Well-child care exams, including routine tests, according to age-based schedule as follows: Nothing, no deductible 20% coinsurance, no deductible • Ten visits during the first year of life • Three visits during the second year of life (age 1 to age 2) • Two visits for age 2 • One visit per calendar year for age 3 and older Routine adult physical exams, including related tests (one per calendar year) Nothing, no deductible 20% coinsurance, no deductible Routine GYN exams, including related lab tests (one per calendar year) Nothing, no deductible 20% coinsurance, no deductible Mental health wellness exams (at least one per calendar year) Nothing, no deductible Nothing, no deductible Routine hearing exams, including routine tests Nothing, no deductible 20% coinsurance, no deductible Hearing aids (up to $2,000 per ear every 36 months for a member age 21 or younger) All charges beyond the 20% coinsurance after deductible maximum after deductible and all charges beyond the maximum Routine vision exams (one every 24 months) Nothing, no deductible 20% coinsurance, no deductible Family planning services—office visits Nothing, no deductible 20% coinsurance, no deductible Outpatient Care Emergency room visits $150 per visit after deductible $150 per visit after deductible (copayment waived if admitted (copayment waived if admitted or for observation stay) or for observation stay) Office or health center visits Nothing after deductible 20% coinsurance after deductible Mental health or substance use treatment Nothing after deductible 20% coinsurance after deductible Outpatient telehealth services • With a covered provider Same as in-person visit Same as in-person visit • With the in-network designated telehealth vendor Nothing after deductible Only applicable in-network Diabetic management services (first two visits per calendar year*) Nothing, no deductible 20% coinsurance after deductible Chiropractors’ office visits Nothing after deductible 20% coinsurance after deductible Acupuncture visits (up to 12 visits per calendar year) Nothing after deductible 20% coinsurance after deductible Short-term rehabilitation therapy—physical and occupational (up to 60 visits per calendar year**) Nothing after deductible 20% coinsurance after deductible Speech, hearing, and language disorder treatment—speech therapy Nothing after deductible 20% coinsurance after deductible Diagnostic x-rays and lab tests, including CT scans, MRIs, PET scans, Nothing after deductible 20% coinsurance after deductible and nuclear cardiac imaging tests Home health care and hospice services Nothing after deductible 20% coinsurance after deductible Oxygen and equipment for its administration Nothing after deductible 20% coinsurance after deductible Durable medical equipment—such as wheelchairs, crutches, hospital beds 20% coinsurance after 40% coinsurance after deductible*** deductible*** Prosthetic devices 20% coinsurance after deductible 40% coinsurance after deductible Surgery and related anesthesia Nothing after deductible 20% coinsurance after deductible Inpatient Care (including maternity care) General or chronic disease hospital care (as many days as medically necessary) Nothing after deductible 20% coinsurance after deductible Mental hospital or substance use facility care (as many days as medically necessary) Nothing after deductible 20% coinsurance after deductible Rehabilitation hospital care (up to 60 days per calendar year) Nothing after deductible 20% coinsurance after deductible Skilled nursing facility care (up to 100 days per calendar year) Nothing after deductible 20% coinsurance after deductible * These diabetic services are for diabetes evaluation and management services, diabetic eye exams, or diabetic foot care. ** No visit limit applies when short-term rehabilitation therapy is furnished as part of covered home health care or for the treatment of autism spectrum disorders. *** In-network cost share waived for one breast pump per birth, including supplies (20% coinsurance after deductible out-of-network).
 Preferred Blue PPO Saver - Summary of Benefits Page 2 Page 4
Preferred Blue PPO Saver - Summary of Benefits Page 2 Page 4