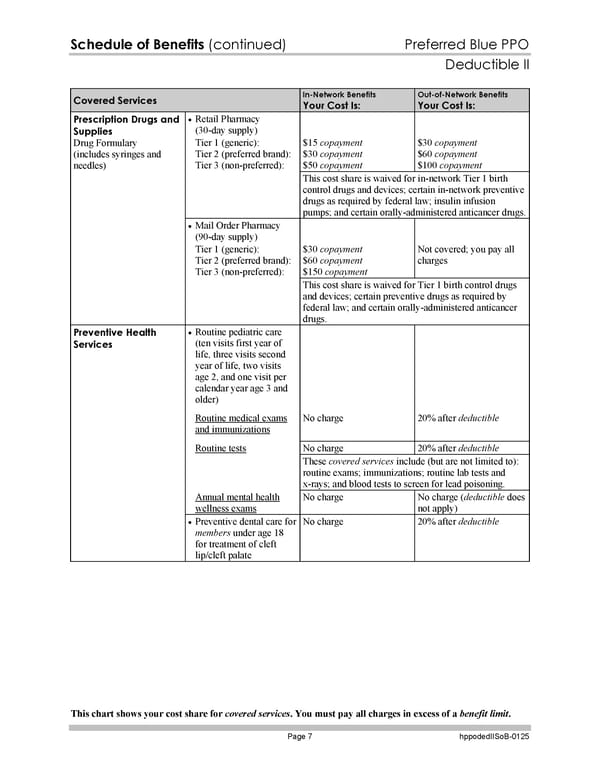
Schedule of Benefits (continued) Preferred Blue PPO Deductible II This chart shows your cost share for covered services. You must pay all charges in excess of a benefit limit. Page 7 hppodedIISoB-0125 Covered Services In-Network Benefits Your Cost Is: Out-of-Network Benefits Your Cost Is: Retail Pharmacy (30-day supply) $15 copayment $30 copayment $50 copayment $30 copayment $60 copayment $100 copayment Tier 1 (generic): Tier 2 (preferred brand): Tier 3 (non-preferred): This cost share is waived for in-network Tier 1 birth control drugs and devices; certain in-network preventive drugs as required by federal law; insulin infusion pumps; and certain orally-administered anticancer drugs. Mail Order Pharmacy (90-day supply) $30 copayment $60 copayment $150 copayment Not covered; you pay all charges Prescription Drugs and Supplies Drug Formulary (includes syringes and needles) Tier 1 (generic): Tier 2 (preferred brand): Tier 3 (non-preferred): This cost share is waived for Tier 1 birth control drugs and devices; certain preventive drugs as required by federal law; and certain orally-administered anticancer drugs. Routine pediatric care (ten visits first year of life, three visits second year of life, two visits age 2, and one visit per calendar year age 3 and older) Routine medical exams and immunizations No charge 20% after deductible No charge 20% after deductible Routine tests These covered services include (but are not limited to): routine exams; immunizations; routine lab tests and x-rays; and blood tests to screen for lead poisoning. Annual mental health wellness exams No charge No charge (deductible does not apply) Preventive Health Services Preventive dental care for members under age 18 for treatment of cleft lip/cleft palate No charge 20% after deductible
 Subscriber Certificate and Rider Documentation Page 133 Page 135
Subscriber Certificate and Rider Documentation Page 133 Page 135