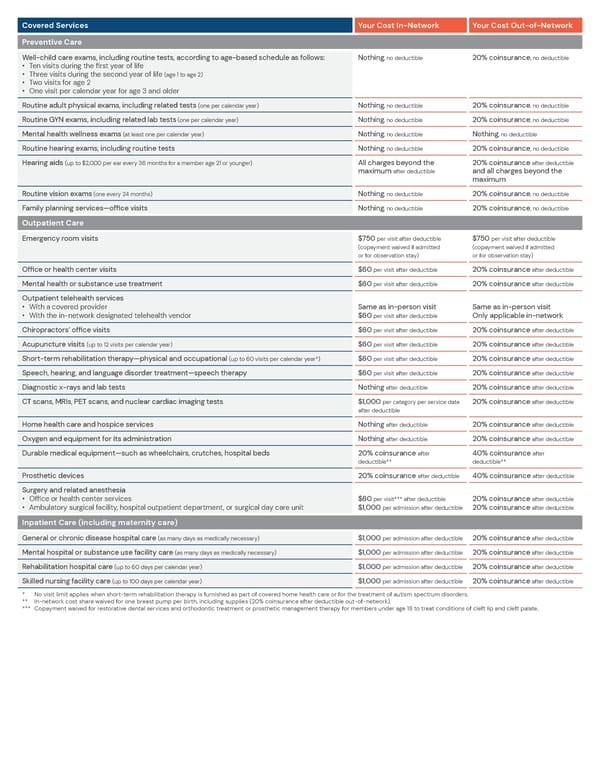
Covered Services Your Cost In-Network Your Cost Out-of-Network Preventive Care Well-child care exams, including routine tests, according to age-based schedule as follows: • Ten visits during the first year of life • Three visits during the second year of life (age 1 to age 2) • Two visits for age 2 • One visit per calendar year for age 3 and older Nothing, no deductible 20% coinsurance, no deductible Routine adult physical exams, including related tests (one per calendar year) Nothing, no deductible 20% coinsurance, no deductible Routine GYN exams, including related lab tests (one per calendar year) Nothing, no deductible 20% coinsurance, no deductible Mental health wellness exams (at least one per calendar year) Nothing, no deductible Nothing, no deductible Routine hearing exams, including routine tests Nothing, no deductible 20% coinsurance, no deductible Hearing aids (up to $2,000 per ear every 36 months for a member age 21 or younger) All charges beyond the maximum after deductible 20% coinsurance after deductible and all charges beyond the maximum Routine vision exams (one every 24 months) Nothing, no deductible 20% coinsurance, no deductible Family planning services—office visits Nothing, no deductible 20% coinsurance, no deductible Outpatient Care Emergency room visits $750 per visit after deductible (copayment waived if admitted or for observation stay) $750 per visit after deductible (copayment waived if admitted or for observation stay) Office or health center visits $60 per visit after deductible 20% coinsurance after deductible Mental health or substance use treatment $60 per visit after deductible 20% coinsurance after deductible Outpatient telehealth services • With a covered provider Same as in-person visit Same as in-person visit • With the in-network designated telehealth vendor $60 per visit after deductible Only applicable in-network Chiropractors’ office visits $60 per visit after deductible 20% coinsurance after deductible Acupuncture visits (up to 12 visits per calendar year) $60 per visit after deductible 20% coinsurance after deductible Short-term rehabilitation therapy—physical and occupational (up to 60 visits per calendar year*) $60 per visit after deductible 20% coinsurance after deductible Speech, hearing, and language disorder treatment—speech therapy $60 per visit after deductible 20% coinsurance after deductible Diagnostic x-rays and lab tests Nothing after deductible 20% coinsurance after deductible CT scans, MRIs, PET scans, and nuclear cardiac imaging tests $1,000 per category per service date after deductible 20% coinsurance after deductible Home health care and hospice services Nothing after deductible 20% coinsurance after deductible Oxygen and equipment for its administration Nothing after deductible 20% coinsurance after deductible Durable medical equipment—such as wheelchairs, crutches, hospital beds 20% coinsurance after deductible** 40% coinsurance after deductible** Prosthetic devices 20% coinsurance after deductible 40% coinsurance after deductible Surgery and related anesthesia • Office or health center services $60 per visit*** after deductible 20% coinsurance after deductible • Ambulatory surgical facility, hospital outpatient department, or surgical day care unit $1,000 per admission after deductible 20% coinsurance after deductible Inpatient Care (including maternity care) General or chronic disease hospital care (as many days as medically necessary) $1,000 per admission after deductible 20% coinsurance after deductible Mental hospital or substance use facility care (as many days as medically necessary) $1,000 per admission after deductible 20% coinsurance after deductible Rehabilitation hospital care (up to 60 days per calendar year) $1,000 per admission after deductible 20% coinsurance after deductible Skilled nursing facility care (up to 100 days per calendar year) $1,000 per admission after deductible 20% coinsurance after deductible * No visit limit applies when short-term rehabilitation therapy is furnished as part of covered home health care or for the treatment of autism spectrum disorders. ** In-network cost share waived for one breast pump per birth, including supplies (20% coinsurance after deductible out-of-network). *** Copayment waived for restorative dental services and orthodontic treatment or prosthetic management therapy for members under age 18 to treat conditions of cleft lip and cleft palate.
 BlueCross BlueShield Preferred Blue PPO Basic Saver Summary Page 2 Page 4
BlueCross BlueShield Preferred Blue PPO Basic Saver Summary Page 2 Page 4