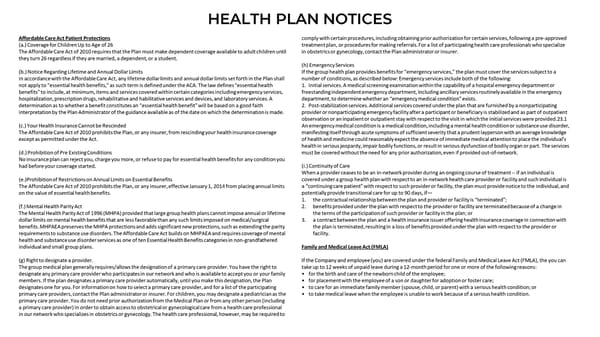
HEALTH PLAN NOTICES Affordable Care Act Patient Protections comply with certain procedures, including obtaining prior authorization for certain services, following a pre-approved (a.) Coverage for Children Up to Age of 26 treatment plan, or procedures for making referrals. For a list of participating health care professionals who specialize The Affordable Care Act of 2010 requires that the Plan must make dependent coverage available to adult children until in obstetrics or gynecology, contact the Plan administrator or Insurer. they turn 26 regardless if they are married, a dependent, or a student. (h) Emergency Services (b.) Notice Regarding Lifetime and Annual Dollar Limits If the group health plan provides benefits for “emergency services,” the plan must cover the services subject to a In accordance with the Affordable Care Act, any lifetime dollar limits and annual dollar limits set forth in the Plan shall number of conditions, as described below: Emergency services include both of the following: not apply to “essential health benefits,” as such term is defined under the ACA. The law defines “essential health 1. Initial services. A medical screening examination within the capability of a hospital emergency department or benefits” to include, at minimum, items and services covered within certain categories including emergency services, freestanding independent emergency department, including ancillary services routinely available in the emergency hospitalization, prescription drugs, rehabilitative and habilitative services and devices, and laboratory services. A department, to determine whether an “emergency medical condition” exists. determination as to whether a benefit constitutes an “essential health benefit” will be based on a good faith 2. Post-stabilization services. Additional services covered under the plan that are furnished by a nonparticipating interpretation by the Plan Administrator of the guidance available as of the date on which the determination is made. provider or nonparticipating emergency facility after a participant or beneficiary is stabilized and as part of outpatient observation or an inpatient or outpatient stay with respect to the visit in which the initial services were provided.23.1 (c.) Your Health Insurance Cannot be Rescinded An emergency medical condition is a medical condition, including a mental health condition or substance use disorder, The Affordable Care Act of 2010 prohibits the Plan, or any insurer, from rescinding your health insurance coverage manifesting itself through acute symptoms of sufficient severity that a prudent layperson with an average knowledge except as permitted under the Act. of health and medicine could reasonably expect the absence of immediate medical attention to place the individual’s health in serious jeopardy, impair bodily functions, or result in serious dysfunction of bodily organ or part. The services (d.) Prohibition of Pre Existing Conditions must be covered without the need for any prior authorization, even if provided out-of-network. No insurance plan can reject you, charge you more, or refuse to pay for essential health benefits for any condition you had before your coverage started. (i.) Continuity of Care When a provider ceases to be an in-network provider during an ongoing course of treatment --if an individual is (e.)Prohibition of Restrictions on Annual Limits on Essential Benefits covered under a group health plan with respect to an in-network health care provider or facility and such individual is The Affordable Care Act of 2010 prohibits the Plan, or any insurer, effective January 1, 2014 from placing annual limits a “continuing care patient” with respect to such provider or facility, the plan must provide notice to the individual, and on the value of essential health benefits. potentially provide transitional care for up to 90 days, if— 1. the contractual relationship between the plan and provider or facility is “terminated”; (f.) Mental Health Parity Act 2. benefits provided under the plan with respect to the provider or facility are terminated because of a change in The Mental Health Parity Act of 1996 (MHPA) provided that large group health plans cannot impose annual or lifetime the terms of the participation of such provider or facility in the plan; or dollar limits on mental health benefits that are less favorable than any such limits imposed on medical/surgical 3. a contract between the plan and a health insurance issuer offering health insurance coverage in connection with benefits. MHPAEA preserves the MHPA protections and adds significant new protections, such as extending the parity the plan is terminated, resulting in a loss of benefits provided under the plan with respect to the provider or requirements to substance use disorders. The Affordable Care Act builds on MHPAEA and requires coverage of mental facility. health and substance use disorder services as one of ten Essential Health Benefits categories in non-grandfathered individual and small group plans. Family and Medical Leave Act (FMLA) (g) Right to designate a provider. If the Company and employee (you) are covered under the federal Family and Medical Leave Act (FMLA), the you can The group medical plan generally requires/allows the designation of a primary care provider. You have the right to take up to 12 weeks of unpaid leave during a 12-month period for one or more of the following reasons: designate any primary care provider who participates in our network and who is available to accept you or your family • for the birth and care of the newborn child of the employee; members. If the plan designates a primary care provider automatically, until you make this designation, the Plan • for placement with the employee of a son or daughter for adoption or foster care; designates one for you. For information on how to select a primary care provider, and for a list of the participating • to care for an immediate family member (spouse, child, or parent) with a serious health condition; or primary care providers, contact the Plan administrator or insurer. For children, you may designate a pediatrician as the • to take medical leave when the employee is unable to work because of a serious health condition. primary care provider. You do not need prior authorization from the Medical Plan or from any other person (including a primary care provider) in order to obtain access to obstetrical or gynecological care from a health care professional in our network who specializes in obstetrics or gynecology. The health care professional, however, may be required to
 Camunda 2023 Employee Benefit Guide Page 23 Page 25
Camunda 2023 Employee Benefit Guide Page 23 Page 25