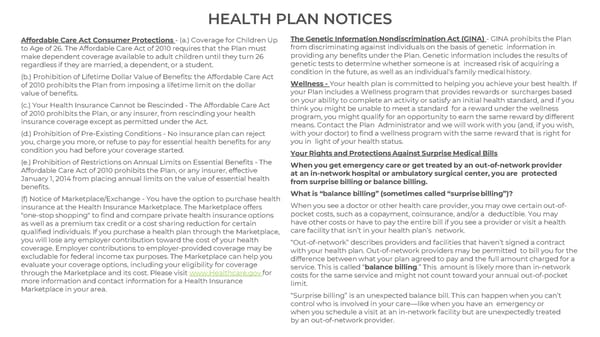
HEALTH PLAN NOTICES Nondiscrimination Act (GINA) - GINA prohibits the Plan Affordable Care Act Consumer Protections - (a.) Coverage for Children Up The Genetic Information to Age of 26. The Affordable Care Act of 2010 requires that the Plan must from discriminating against individuals on the basis of genetic information in make dependent coverage available to adult children until they turn 26 providing any benefits under the Plan. Genetic information includes the results of regardless if they are married, a dependent, or a student. genetic tests to determine whether someone is at increased risk of acquiring a (b.) Prohibition of Lifetime Dollar Value of Benefits: the Affordable Care Act condition in the future, as well as an individual’s family medical history. of 2010 prohibits the Plan from imposing a lifetime limit on the dollar Wellness - Your health plan is committed to helping you achieve your best health. If value of benefits. your Plan includes a Wellness program that provides rewards or surcharges based (c.) Your Health Insurance Cannot be Rescinded - The Affordable Care Act on your ability to complete an activity or satisfy an initial health standard, and if you of 2010 prohibits the Plan, or any insurer, from rescinding your health think you might be unable to meet a standard for a reward under the wellness insurance coverage except as permitted under the Act. program, you might qualify for an opportunity to earn the same reward by different means. Contact the Plan Administrator and we will work with you (and, if you wish, (d.) Prohibition of Pre-Existing Conditions - No insurance plan can reject with your doctor) to find a wellness program with the same reward that is right for you, charge you more, or refuse to pay for essential health benefits for any you in light of your health status. condition you had before your coverage started. Your Rights and Protections Against Surprise Medical Bills (e.) Prohibition of Restrictions on Annual Limits on Essential Benefits - The When you get emergency care or get treated by an out-of-network provider Affordable Care Act of 2010 prohibits the Plan, or any insurer, effective at an in-network hospital or ambulatory surgical center, you are protected January 1, 2014 from placing annual limits on the value of essential health from surprise billing or balance billing. benefits. What is “balance billing” (sometimes called “surprise billing”)? (f) Notice of Marketplace/Exchange - You have the option to purchase health insurance at the Health Insurance Marketplace. The Marketplace offers When you see a doctor or other health care provider, you may owe certain out-of- "one-stop shopping" to find and compare private health insurance options pocket costs, such as a copayment, coinsurance, and/or a deductible. You may as well as a premium tax credit or a cost sharing reduction for certain have other costs or have to pay the entire bill if you see a provider or visit a health qualified individuals. If you purchase a health plan through the Marketplace, care facility that isn’t in your health plan’s network. you will lose any employer contribution toward the cost of your health “Out-of-network” describes providers and facilities that haven’t signed a contract coverage. Employer contributions to employer-provided coverage may be with your health plan. Out-of-network providers may be permitted to bill you for the excludable for federal income tax purposes. The Marketplace can help you difference between what your plan agreed to pay and the full amount charged for a evaluate your coverage options, including your eligibility for coverage service. This is called “balance billing.” This amount is likely more than in-network for through the Marketplace and its cost. Please visit www.Healthcare.gov costs for the same service and might not count toward your annual out-of-pocket more information and contact information for a Health Insurance limit. Marketplace in your area. “Surprise billing” is an unexpected balance bill. This can happen when you can’t control who is involved in your care—like when you have an emergency or when you schedule a visit at an in-network facility but are unexpectedly treated by an out-of-network provider.
 CIEE 2024 Employee Benefit Guide Page 35 Page 37
CIEE 2024 Employee Benefit Guide Page 35 Page 37