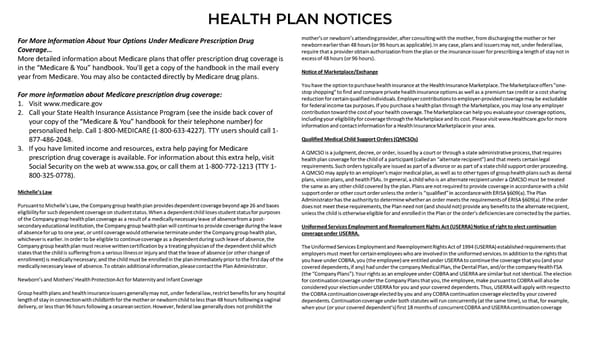
HEALTH PLAN NOTICES For More Information About Your Options Under Medicare Prescription Drug mother’s or newborn’s attending provider, after consulting with the mother, from discharging the mother or her Coverage… newborn earlier than 48 hours (or 96 hours as applicable). In any case, plans and issuers may not, under federal law, require that a provider obtain authorization from the plan or the insurance issuer for prescribing a length of stay not in More detailed information about Medicare plans that offer prescription drug coverage is excess of 48 hours (or 96 hours). in the “Medicare & You” handbook. You’ll get a copy of the handbook in the mail every Notice of Marketplace/Exchange year from Medicare. You may also be contacted directly by Medicare drug plans. You have the option to purchase health insurance at the Health Insurance Marketplace. The Marketplace offers "one- For more information about Medicare prescription drug coverage: stop shopping" to find and compare private health insurance options as well as a premium tax credit or a cost sharing 1. Visit www.medicare.gov reduction for certain qualified individuals. Employer contributions to employer-provided coverage may be excludable for federal income tax purposes. If you purchase a health plan through the Marketplace, you may lose any employer 2. Call your State Health Insurance Assistance Program (see the inside back cover of contribution toward the cost of your health coverage. The Marketplace can help you evaluate your coverage options, your copy of the “Medicare & You” handbook for their telephone number) for including your eligibility for coverage through the Marketplace and its cost. Please visit www.Healthcare.gov for more personalized help. Call 1-800-MEDICARE (1-800-633-4227). TTY users should call 1- information and contact information for a Health Insurance Marketplace in your area. 877-486-2048. Qualified Medical Child Support Orders (QMCSOs) 3. If you have limited income and resources, extra help paying for Medicare A QMCSO is a judgment, decree, or order, issued by a court or through a state administrative process, that requires prescription drug coverage is available. For information about this extra help, visit health plan coverage for the child of a participant (called an “alternate recipient”) and that meets certain legal Social Security on the web at www.ssa.gov, or call them at 1-800-772-1213 (TTY 1- requirements. Such orders typically are issued as part of a divorce or as part of a state child support order proceeding. 800-325-0778). A QMCSO may apply to an employer's major medical plan, as well as to other types of group health plans such as dental plans, vision plans, and health FSAs. In general, a child who is an alternate recipient under a QMCSO must be treated the same as any other child covered by the plan. Plans are not required to provide coverage in accordance with a child Michelle’s Law support order or other court order unless the order is “qualified” in accordance with ERISA §609(a). The Plan Administrator has the authority to determine whether an order meets the requirements of ERISA §609(a). If the order Pursuant to Michelle’s Law, the Company group health plan provides dependent coverage beyond age 26 and bases does not meet these requirements, the Plan need not (and should not) provide any benefits to the alternate recipient, eligibility for such dependent coverage on student status. When a dependent child loses student status for purposes unless the child is otherwise eligible for and enrolled in the Plan or the order's deficiencies are corrected by the parties. of the Company group health plan coverage as a result of a medically necessary leave of absence from a post- secondary educational institution, the Company group health plan will continue to provide coverage during the leave Uniformed Services Employment and Reemployment Rights Act (USERRA) Notice of right to elect continuation of absence for up to one year, or until coverage would otherwise terminate under the Company group health plan, coverage under USERRA. whichever is earlier. In order to be eligible to continue coverage as a dependent during such leave of absence, the Company group health plan must receive written certification by a treating physician of the dependent child which The Uniformed Services Employment and Reemployment Rights Act of 1994 (USERRA) established requirements that states that the child is suffering from a serious illness or injury and that the leave of absence (or other change of employers must meet for certain employees who are involved in the uniformed services. In addition to the rights that enrollment) is medically necessary; and the child must be enrolled in the plan immediately prior to the first day of the you have under COBRA, you (the employee) are entitled under USERRA to continue the coverage that you (and your medically necessary leave of absence. To obtain additional information, please contact the Plan Administrator. covered dependents, if any) had under the company Medical Plan, the Dental Plan, and/or the company Health FSA (the “Company Plans”). Your rights as an employee under COBRA and USERRA are similar but not identical. The election Newborn’s and Mothers’ Health Protection Act for Maternity and Infant Coverage for continuation coverage under the Company Plans that you, the employee, make pursuant to COBRA will also be considered your election under USERRA for you and your covered dependents. Thus, USERRA will apply with respect to Group health plans and health insurance issuers generally may not, under federal law, restrict benefits for any hospital the COBRA continuation coverage elected by you and any COBRA continuation coverage elected by your covered length of stay in connection with childbirth for the mother or newborn child to less than 48 hours following a vaginal dependents. Continuation coverage under both statutes will run concurrently (at the same time), so that, for example, delivery, or less than 96 hours following a cesarean section. However, federal law generally does not prohibit the when your (or your covered dependent’s) first 18 months of concurrent COBRA and USERRA continuation coverage
 Camunda 2023 Employee Benefit Guide Page 26 Page 28
Camunda 2023 Employee Benefit Guide Page 26 Page 28